Your Cart is Empty

November 28, 2023 8 min read
Take our quiz and find which supplements your body is craving.

While menopause is a more talked about, prominent topic when it comes to female health issues, that is not the case with perimenopause. An initial stage in the (often rocky) menopausal transition, the perimenopause experience is just as unique as any other bodily process. For some women, it can be pretty much non-existent, while for others, it might be quite intense and challenging.
Contrary to popular belief, perimenopause isn’t always a short stage leading up to menopause. In fact, onset can begin as early as the mid-thirties, and it can last for years, triggering unpleasant, sometimes even debilitating symptoms - both physical and psychological.
In an attempt to lift the veil off this critical healthcare issue and raise greater awareness around early perimenopause, we will dive into its early symptoms, the hormonal changes that accompany it, and potential treatments that could help. Keep reading to learn more!
Before we can fully understand perimenopause, we must dive into the complexity of the menopausal transition and all menopausal stages. Menopause is, by definition, a process that begins with a 12-month absence of the menstrual period. While it usually occurs when a woman enters her 50s, it can also begin in their 40s for some women.[1]
However, the menopausal transition is not necessarily a linear process. It is preceded by perimenopause, which is characterized by irregular periods, hot flashes, sudden mood swings, a slower metabolism, and night sweats.[1] Sounds familiar? That’s right - it is perfectly normal for women to experience menopausal symptoms before menopause itself even starts.
One of the primary changes indicating the start of menopause is a significant decline in estrogen levels. Given that estrogen plays a vital role in female reproductive health, the effects of this decline can be rather drastic. Estrogen controls the menstrual cycle but plays numerous other noteworthy roles, too. It affects the proper functioning of the reproductive tract, urinary tract, heart, blood vessels, skin, hair, pelvic muscles, bones, and brain![2]
Low estrogen levels can lead to irregular periods, high cholesterol, bone health issues such as osteoporosis, decreased libido, and even cardiovascular problems. As we’ve mentioned, perimenopausal and menopausal changes aren’t identical for all women, and they can range from mild to life-altering.[3]

In a nutshell, the menopausal stages[4] go as follows:
Perimenopause, the initial phase of the menopausal process, is often a preview of what awaits once menopause kicks in. However, for many women, perimenopause is far more than just a glimpse of menopausal symptoms. It can be pretty intense, and to make matters worse, it can start prematurely - as early as the mid-30s!
Perimenopause comes from the Greek word peri,meaning “about.” That being said, perimenopause should occur around actual menopause, but for some women, it sneaks up years ahead of its time.[5]
Remember how we said that, as we age, estrogen levels drop, causing a series of adverse health effects? It is during perimenopause that this primary female hormone experiences rather drastic fluctuations, resulting in menstrual irregularity and changes in both menstrual cycle longevity and accompanying symptoms.[5]

What’s more, perimenopausal women may experience menstrual cycles with no ovulation - meaning an egg isn’t released. Therefore, perimenopause, or the stage preceding menopause, may be perceived as the body’s method of gradually anticipating and adjusting to the upcoming changes.
One of the first tell-tale signs that you’re experiencing perimenopause are irregular periods. You may notice that your menstrual periods have become longer or shorter. Even if you haven’t experienced changes in flow before, they may occur in this stage. However, these changes aren’t always constant and don’t necessarily manifest every month.[5]
It is common for perimenopausal women to skip periods, but the severity of changes in your menstrual cycle can indicate if you’re in early or late menopause. For instance, getting your period seven days earlier or later may signify that you’ve just entered perimenopause - especially if you haven’t experienced it before. On the other hand, not getting your period for two consecutive months or more is likely a sign of late perimenopause.[5]
Mood swings often accompany all three menopausal stages. Increased irritability, depressive moods, and anxiety are often experienced in perimenopause, especially as a result of other unpleasant physical symptoms. Many women experience irritability as a result of poor sleep hygiene. Sleep is typically compromised during perimenopause, as hot flashes and night sweats create a rather uncomfortable atmosphere for achieving optimal rest.[5]

Hot flashes are certainly one of the leading associations with menopause and one of the most prominent symptoms of all three menopausal stages. This sudden rush of warmth felt in the upper body, followed by intense sweating, usually lasts a few minutes. Hot flashes are followed by a rapid heartbeat, restlessness, and a sudden drop in bodily temperature once they’re over, which may give you the chills.[6]
Hormonal changes also affect tissue tone and plasticity, resulting in vaginal dryness and urinary incontinence. In addition to being more prone to urinary and vaginal infections, women may experience painful intercourse. These physical symptoms, intertwined with irritability, anxiety, and depressive moods, may also affect sexual desire.[5]
Altered menstrual cycle and ovulation periods go hand in hand with decreased fertility, which is one of the most drastic consequences of perimenopause. It is, however, essential to note that pregnancy is still possible as long as you’re having periods - no matter how irregular they may be.[5]
Low estrogen equals an increased risk of fragile bones and conditions such as osteoporosis. The lack of estrogen may also increase LDL cholesterol (the “bad”cholesterol) in the blood, increasing the chance of cardiovascular issues. In addition to the increase in bad cholesterol, perimenopausal women also face a decrease in HDL cholesterol - the so-called “good” cholesterol, which also jeopardizes heart health.[5]
Why is it that some women start experiencing these symptoms as early as their mid to late thirties? Premature menopause is diagnosed in women under 40, while early menopause begins between the ages of 40 and 45 and affects 12% of women.[7] Here’s why it may happen:

Yes, both perimenopause and menopause are natural, inevitable processes. But does that mean we just have to go with the flow and accept our fate when it comes to their exhausting, life-altering side effects? The truth is that nutritional choices can significantly alleviate these symptoms, and certain dietary supplements may make the transition a lot smoother.
We’ve already mentioned how low estrogen levels may jeopardize bone density, leading to degenerative conditions during perimenopause and menopause. Vitamin D plays a crucial role in bone metabolism and calcium production. It is also a key factor in cardiovascular health and may help alleviate emotional and psychological symptoms accompanying this phase.[8] The vitamin D3+K2 combo promotes calcium absorption and integration, which is extremely important in perimenopause.
Omega-3 fatty acids represent a staple in female health in all its stages, including menstrual pain, pregnancy, breastfeeding, as well as perimenopause and menopause. Supplementing with omega-3s can improve mood levels during menopausal transition by reducing both depressive symptoms as well as vasomotor symptoms (VMS) - also known as hot flashes.[9]
Probiotics are a must in every supplement stack and are crucial to gut health, immune strength, and mental health. A quality probiotic supplement could improve the cardiometabolic health of perimenopausal women while also helping you balance out your hormones.[10]
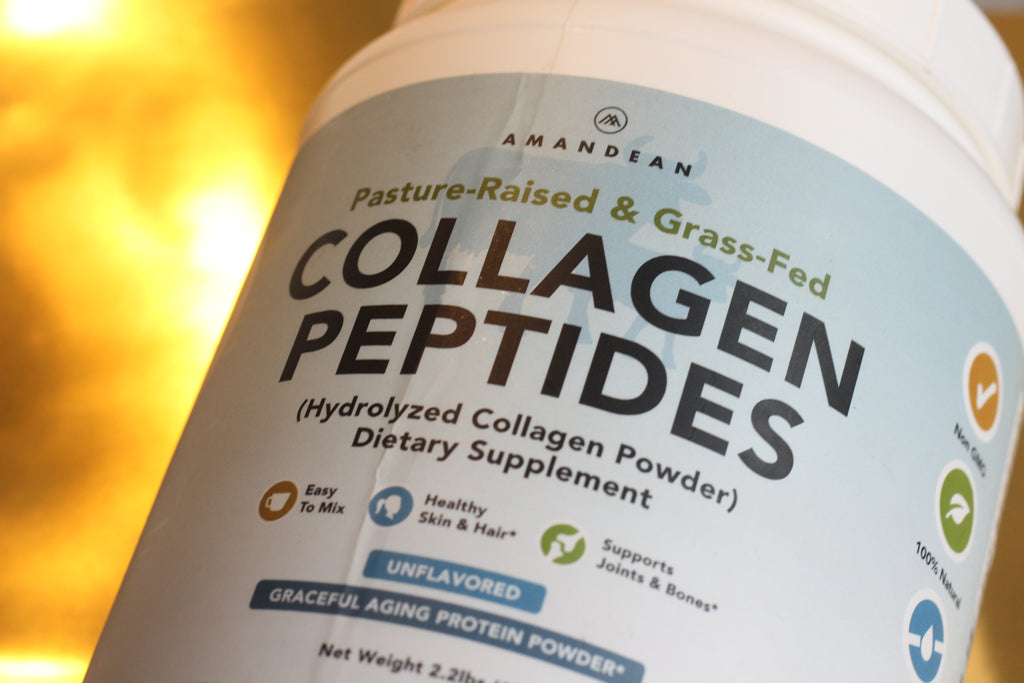
The multifaceted role of collagen in female health, especially during perimenopause and menopause, makes it one of the essential supplements for this important stage of your life. Collagen, the main structural protein in our body, is produced naturally, but this production significantly decreases as we age.
Collagen plays a key role in skin health, and it can dramatically improve symptoms of dermatoporosis - a common skin condition in perimenopause and menopause.[11] Collagen also preserves bone density, which we’ve already established is a burning topic in the menopausal transition.[12]
While certain bodily processes that accompany aging cannot be stopped or avoided, their symptoms and side effects can certainly be managed wisely. We don’t get to decide when perimenopause or menopause will arrive, as they’re completely unique to every individual. We can, however, make certain adjustments and opt for natural supplementation to ease the unpleasant symptoms, in addition to adopting a healthy diet and prioritizing physical activity. Learn more about making healthier dietary choices and optimizing your lifestyle, and discover non-GMO, all-natural supplementation.

March 20, 2025 8 min read
Discover the benefits of creatine for women with Amandean’s Creatine HCI. Improve strength, energy, recovery, and cognitive function with this high-absorption formula. Its advanced HCl form ensures easy digestion and no bloating, providing all the benefits without the drawbacks. Elevate your fitness journey and overall wellness with a supplement designed for women’s unique needs.

March 03, 2025 7 min read
Discover how Bryan Johnson, a tech entrepreneur turned biohacker, uses cutting-edge science and personalized genetic testing to revolutionize health and longevity. Learn how biohacking, from diet to mental health practices, can help you live longer and healthier, with practical strategies to optimize your well-being. Find out more about genetic testing, and ways to implement results into your wellness routine.

February 19, 2025 6 min read
Explore the remarkable health benefits of medicinal mushrooms like Lion’s Mane, Turkey Tail, Chaga, and Reishi. These superplants support immune function, reduce inflammation, and boost brain health. Learn about Amandean's Brain Health supplement, combining Lion’s Mane, Magtein, and Alpha-GPC for optimal cognitive performance.